Tag Archive for: Juvederm

HPV and Cancer: How Are They Connected?
Human papillomavirus (HPV) is the most common sexually transmitted infection (STI) within the United States. It infects more than 40 million individuals, usually those in their late teens and early 20s, each year. However, these numbers…
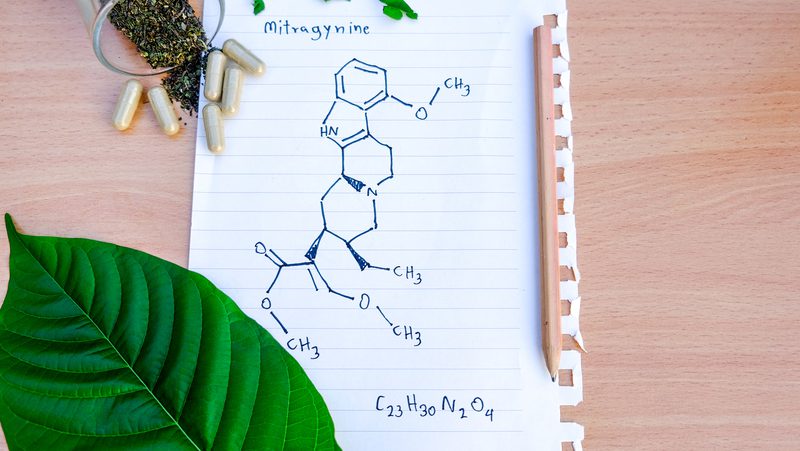
Kava and Kratom: Benefits and Differences
While society is placing a growing emphasis on “natural†ingredients, this is often a misleading term as most assume that natural, plant-derived ingredients are safe and healthy. However, that is not always the…

O-Shot® for Improving the Female Orgasm
For women struggling to orgasm, and not for lack of effort on their partner’s part, things can seem immensely frustrating. Or, maybe you can orgasm, but it is a significant letdown and not as satisfying as you expected. Whatever…
P-Shot® for Erectile Dysfunction and Prevention
As a man engaging in intimate activities with a partner, few things are more frustrating than realizing that your body has not gotten the memo about where you would like things to progress to, or for you to be in the middle of “getting…

Semaglutide for Weight Loss: Facts, Benefits, and Risks
Weight is a common concern and struggle in modern-day society, with many people trying to lose weight but making no progress despite their best efforts. In addition to the impact excess weight leaves on your self-esteem, it is also a common…

Vitamins And Supplements That Increase Vaginal Lubrication
Vaginal dryness is an unpleasant condition, and while it is most often associated with menopausal women, it can affect women at any age, with anxiety, stress, and dehydration common factors causing decreased lubrication.
In addition to being…
Unmasking Testosterone
Testosterone replacement therapy, a vital treatment for restoring balance to declining hormone levels, is being vastly underused. Besides the stigma surrounding hormone replacement therapy, one of the primary reasons for this is that many people…
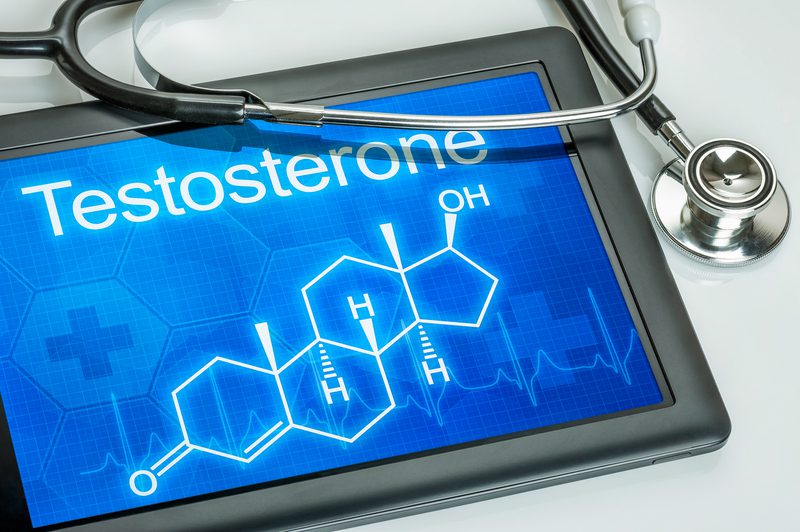
Testosterone Replacement Therapy in Men Under 30
The hormones in our body play a powerful role in many actions, but that doesn’t mean that they always stay at the level we need them. Some natural decline in hormones is expected as we age, but in some cases, this decline…

COVID-19 And Its Potential Effect to Hormones
After two years of COVID-19 exposure, many of us feel as though we know what happens with this infection. It attacks the respiratory system, causes a nasty-sounding cough, and can leave people unbelievably fatigued.
However, as research…

The Relationship Between Inflammation and Sugar Consumption
Inflammation is a natural component of the immune system that aids the body through its healing process. However, certain foods, such as sugar, can cause inflammation in the body. While this is normal, over-consumption of sugar can lead to…
